 |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Completing a Suicide Risk ScreenTherapists need to complete a suicide risk screen when themes of suicidality are evident during interaction with a client.This includes if the client presented thoughts of suicide in a passive statement such as:
This also includes if the client reports thoughts of suicide that have increased in frequency and/or intensity. The purpose of the suicide risk screen is to determine the THOUGHTS / PLAN / INTENT of suicide specific to this client at this point in time. Therapists are encouraged to use the suicide risk screener tool to help elicit information. View the risk screening tool at SAK Suicide Risk Screener |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Action Following Risk Screening
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
If a client is identified as a HIGH level risk (red)
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Mental Health Assessment Team Contact DetailsContact details for local mental health assessment teams Australia wide:
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Victoria Regional Contact DetailsContact details for Victorian geographical areas are as per the following website:http://www.health.vic.gov.au/mentalhealthservices
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Victoria Paediatric / Youth Services
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|||||||||||||||||||||||||||||||||||
|
|
|||||||||||||||||||||||||||||||||||
|
Completing a Suicide Risk ScreenTherapists need to complete a suicide risk screen when themes of suicidality are evident during interaction with a client – even when the client is a child or adolescent.This includes if the client presented thoughts of suicide in a passive statement such as:
Consideration for screening suicide risk in children and young people. See below risk factors and warning signs to consider:
This also includes if the client reports thoughts of suicide that have increased in frequency and/or intensity. The purpose of the suicide risk screen is to determine the THOUGHTS / PLAN / INTENT of suicide specific to this client at this point in time. Therapists are encouraged to use the suicide risk screener tool to help elicit information. View the risk screening tool at SAK Suicide Risk Screener Therapists are encouraged to adapt their language to meet the client’s individual needs and developmental level. |
|||||||||||||||||||||||||||||||||||
|
Action Following Risk Screening
|
|||||||||||||||||||||||||||||||||||
|
|
|||||||||||||||||||||||||||||||||||
|
|
|||||||||||||||||||||||||||||||||||
|
Appendix 1 – Mental health support line
|
|||||||||||||||||||||||||||||||||||
|
Appendix 2 - Child and adolescent mental health service (CAMHS or CYMHS) crisis contact numbers
|
|||||||||||||||||||||||||||||||||||
|
Victoria Regional Contact DetailsContact details for Victorian geographical areas are as per the following website:http://www3.health.vic.gov.au/mentalhealthservices/child/index.htm
|
|||||||||||||||||||||||||||||||||||
 |
|
|
Identifying RiskIf a client tells you they have recently self-harmed or you notice a client may have self-injured complete the following screen.
Explore why the client has self-harmed so you can ensure any problems are dealt with. What led up to the self-injury? |
|
|
Self-Harm Risk Screening
|
|
|
Next StepsIf after going through these steps, the client is threatening self-injury or they are at risk of further self-injury and do not have support in place to assist with this.
|
|
|
Following Contact with Client
|
|
|
Complete Pre-Assessment Risk Screen PRIOR to any further clinical activity with client |
 |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Part 1: Identifying RiskIf a client tells you they have recently self-injured or you notice a client may have self-injured complete the following screen:
Where appropriate, ask the client directly in relation to their self-injury. If this is not possible, speak with the person who knows the client best. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Part 2: Self-injury risk screening
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Part 3: Action planThe following visual diagram can be used to understand a client’s risk in relation to their self-injury and assist in formulating an action plan.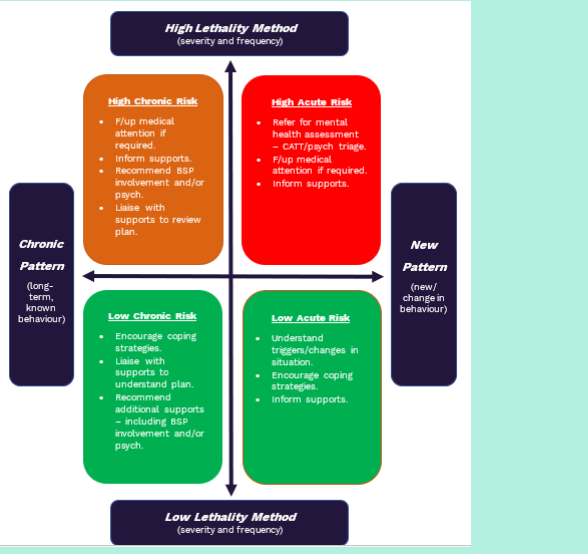
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
High acute risk response (high severity and lethality of behaviour and a new pattern/change in behaviour):
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
High chronic risk response (high severity and lethality of behaviour and a chronic/long-term behaviour with adequate positive behaviour support and/or mental health supports in place)
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Low chronic risk response
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Low acute risk response
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|||||||||||
|
Warning SignsSTAMP can be used to describe behaviours exhibited by a person who is becoming agitated and potentially aggressive and violent.https://www.youthaodtoolbox.org.au/5-recognising-warning-signs-potential-aggressive-behaviour-violence
Additional warning signs could include:
|
|||||||||||
|
Potential Triggers
Antonacci DJ, Manuel C, Davis E. Diagnosis and treatment of aggression in individuals with developmental disabilities. The Psychiatric Quarterly. 2008 Sep;79(3):225-247. DOI: 10.1007/s11126-008-9080-4. |
|||||||||||
|
De-escalation Strategies
|
|||||||||||
 |
|
|
If a therapist attends an appointment and a client has a behaviour of concern. |
|
|
If the client has a BSP
|
|
|
If the client does not have a BSP
|
 |
|
|
Abuse can be defined as the "violation of an individual's human or civil rights, through the act or actions of another person or person" (NDIS, 2022). Example of abuse could include:
|
|
|
If clinicians have concerns regarding abuse and neglect they should always seek assistance from their clinical or team leader for support. As a guide: |
|
|
If a clinician witnesses or receives firsthand reports of events that could be identified as abuse or neglect:
|
|
|
If a clinician is provided information that is not firsthand of events that could be identified as abuse or neglect :
|
|
|
Reporting Contacts
NDIS Participants:
Aged Care:
|
 |
|
|
National 360's Incident and Near Miss Policy and Procedure outlines that your Team Leader / Manager must be informed of all incidents as soon as they occur. The incident Report form should be completed and submitted within 24 hours of the incident occurring. |
|
|
Understanding what incidents require reporting:All therapists are responsible for understanding incident reporting.Clinical Incident: Any acts, omissions, events, or circumstances connected with providing support or services to a person with a disability which have, or could have, caused harm to the person receiving services. Reportable Incident: A reportable incident is any of the below:
WHS Incident: Means a death, serious injury, illness, dangerous incident or near miss that arises out of the conduct of services, whether or not it is reportable to the relevant workplace health and safety regulator. Notifiable Incident: A notifiable incident is when:
|
|
|
What to do when an incident occurs during an appointment:
|
|
|
What to do after the appointment:
|
 |
|
|
Employee Assistance Program (EAP)National 360's EAP program is supported by Psychology Melbourne. You can contact Psychology Melbourne for a confidential discussion to get assistance with any issues related to work, finances, relationships, and family.Phone: 03 9629 1001 Website: www.psychologymelbourne.com.au |
|
|
Suicide Call Back ServiceAnyone thinking about suicide.Website: suicidecallbackservice.org.au Phone: 1300 659 467 |
LifelineAnyone having a personal crisis.Website: www.lifeline.org.au Phone: 13 11 14 |
|
Beyond BlueAnyone feeling anxious or depressed.Website: beyondblue.org.au Phone: 1300 22 46 36 |
Kids HelplineCounselling for young people aged 5-25.Website: kidshelpline.com.au Phone: 1800 55 1800 |
|
MensLine AustraliaMen with emotional or relationship concerns.Website: mensline.org.au Phone: 1300 78 99 78 |
Open ArmsVeterans and families councelling.Website: openarms.gov.au Phone: 1800 011 046 |
 |
|
|
AdvocacyEasy Read: Advocacy |
Complaints and FeedbackEasy Read: Complaints and Feedback |
|
Privacy and Personal InformationEasy Read: Privacy and Personal Information |
What are your Rights?Easy Read: What are your Rights? |
|
Service AgreementsEasy Read: What is a Service Agreement? |
Therapy Plans and Support PlanningEasy Read: Therapy Plans and Support Planning |
|
Withdrawal of ServicesEasy Read: Withdrawal of Services |
BillingEasy Read: Billing |